2025 Advance Notice: CMS Proposes Major Changes to Medicare Advantage and Part D
Related Articles: 2025 Advance Notice: CMS Proposes Major Changes to Medicare Advantage and Part D
- 22025 Seagull Street: A Coastal Paradise In Rodanthe, North Carolina
- November 2025 Holiday Calendar
- Section 202 CrPC: Examination Of Accused By Medical Practitioner
- Celebrating The Year Of The Rabbit: A Comprehensive Guide To Chinese New Year 2025
- When Is Easter Monday 2025?
Introduction
With enthusiasm, let’s navigate through the intriguing topic related to 2025 Advance Notice: CMS Proposes Major Changes to Medicare Advantage and Part D. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Video about 2025 Advance Notice: CMS Proposes Major Changes to Medicare Advantage and Part D
2025 Advance Notice: CMS Proposes Major Changes to Medicare Advantage and Part D

Introduction
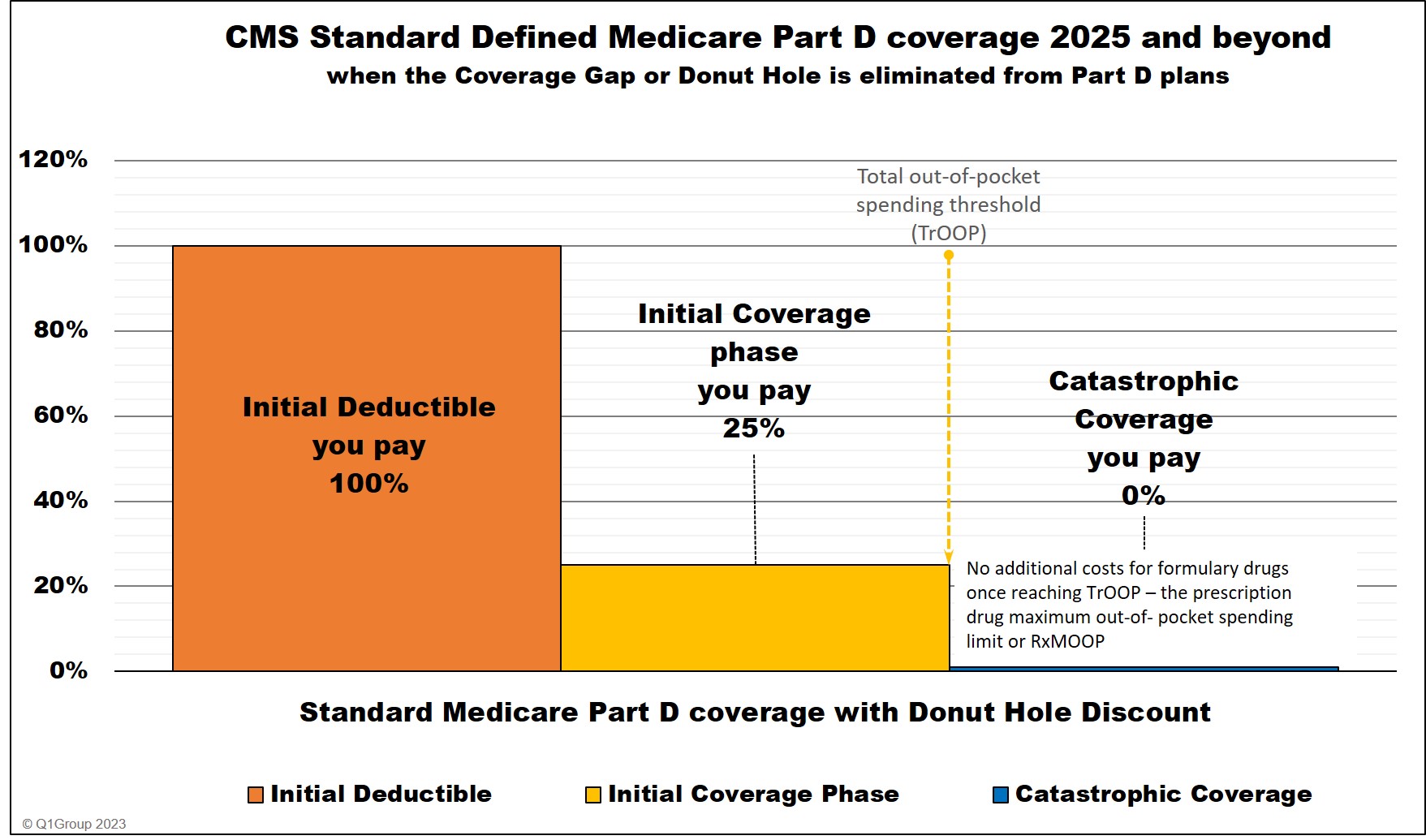
On March 9, 2023, the Centers for Medicare & Medicaid Services (CMS) released its proposed 2025 Advance Notice for Medicare Advantage (MA) and Part D prescription drug plans. This proposed rule, which would take effect on January 1, 2025, represents the most significant changes to the Medicare Advantage program in over a decade. The proposed changes aim to improve the quality of care for beneficiaries, reduce costs, and increase transparency.
Key Proposed Changes
The proposed rule includes a wide range of changes, including:
- New Quality Measures: CMS proposes to add 20 new quality measures to the MA and Part D programs. These measures focus on improving outcomes for beneficiaries with chronic conditions, such as diabetes, heart disease, and cancer.
- Enhanced Star Ratings: CMS proposes to enhance the MA and Part D Star Ratings system to better reflect the quality of care provided by plans. The new system would include more measures related to beneficiary experience and health equity.
- New Payment Model: CMS proposes to implement a new payment model for MA plans that would reward plans for providing high-quality care and improving outcomes for beneficiaries. The new model would replace the current fee-for-service payment system.
- Increased Transparency: CMS proposes to increase transparency in the MA and Part D programs by requiring plans to provide more information to beneficiaries about their coverage and costs. This information would be available on a new online portal.
Impact on Beneficiaries
The proposed changes are expected to have a significant impact on Medicare beneficiaries. The new quality measures and enhanced Star Ratings system will help beneficiaries to identify plans that provide high-quality care. The new payment model will incentivize plans to focus on improving outcomes for beneficiaries. The increased transparency will help beneficiaries to make more informed decisions about their coverage.
Impact on Plans
The proposed changes will also have a significant impact on MA and Part D plans. The new quality measures will require plans to invest in improving the quality of care they provide. The new payment model will change the way that plans are paid for providing care. The increased transparency will make it more difficult for plans to hide information from beneficiaries.
Timeline for Implementation
The proposed rule is open for public comment until May 8, 2023. CMS will then review the comments and issue a final rule later this year. The changes would take effect on January 1, 2025.
Conclusion
The proposed 2025 Advance Notice is a major step forward in improving the quality of care for Medicare beneficiaries. The changes will make it easier for beneficiaries to find plans that provide high-quality care, and they will incentivize plans to focus on improving outcomes for beneficiaries. The increased transparency will help beneficiaries to make more informed decisions about their coverage.



Closure
Thus, we hope this article has provided valuable insights into 2025 Advance Notice: CMS Proposes Major Changes to Medicare Advantage and Part D. We hope you find this article informative and beneficial. See you in our next article!